Tips for successful rehabilitation after supination trauma
Sports injuries to the ankle are among the most common injuries in sports, particularly sprains or ligament tears resulting from supination trauma (Fong et al., 2007).
This results in two challenges. First, after an ankle injury, the risk of re-injury increases, especially in the first 6-12 months (Gribble et al., 2016). Second, few injured individuals receive adequate physical therapy care, which results in difficulty successfully returning to sport and increases the risk of re-injury (Feger et al., 2017).
Related to this is the development of chronic ankle instability, which can occur in up to 40% of individuals after an initial injury (Doherty et al., 2016). Chronic ankle instability is said to occur when unsteadiness, re-ankling, swelling, pain, limited range of motion, or weakened muscles continue to be present one year after the initial injury (Picot et al., 2022).
Based on this data, we recommend physiotherapeutic rehabilitation to successfully return to sports, daily life and work after ankle injuries.
In addition to the injury and the time frame of wound healing. Is the most important step the setting of individual goals, selection of appropriate testing and treatment planning based on this (Tassignon et al., 2019, Wikstrom et al., 2020). If this does not happen, the risk of long-term consequences such as mechanical instability, re-injury, and chronic instability increases (Vuurberg et al., 2018). In addition to preparation for return to competition, testing of various functions is particularly useful for therapy planning. The test results help to identify existing weaknesses or already pronounced strengths and consequently to choose the next steps (Picot et al., 2022).
Key factors in the return to sport process include pain level, swelling, and temperature from the onset (Wikstrom et al., 2020). In addition, validated questionnaires make current functioning and subjective feelings of safety measurable (Picot et al., 2022).
The early phase of training focuses on regaining stability. Improvements should be made, especially in the first 6-12 weeks, to minimize the risk of re-injury. In this phase, milestones target neuromuscular control. This includes testing static and dynamic balance, as well as regaining full range of motion (Tassignon et al., 2019).
As soon as an adequate strength level has been reached, the focus is then on higher-intensity stress tests. Important criteria are movement control and movement quality (Tassignon et al., 2019). Toward the end of rehab, endurance and sport-specific loads become the focus. Tests, individually adapted to the sport, are on the schedule. (Tassignon et al., 2019, Wikstrom et al., 2020).
In addition to physical abilities, mental readiness to return full weight to the ankle also plays an important role in the rehabilitation process. In addition to trusting conversations between therapist and athlete, standardized questionnaires are used to determine these values (Picot et al., 2022, Tassignon et al., 2019, Wikstrom et al., 2020).
The next figures show examples of testing ankle stability (Picot et al., 2022):
Y-balance test (Picot et al., 2022)
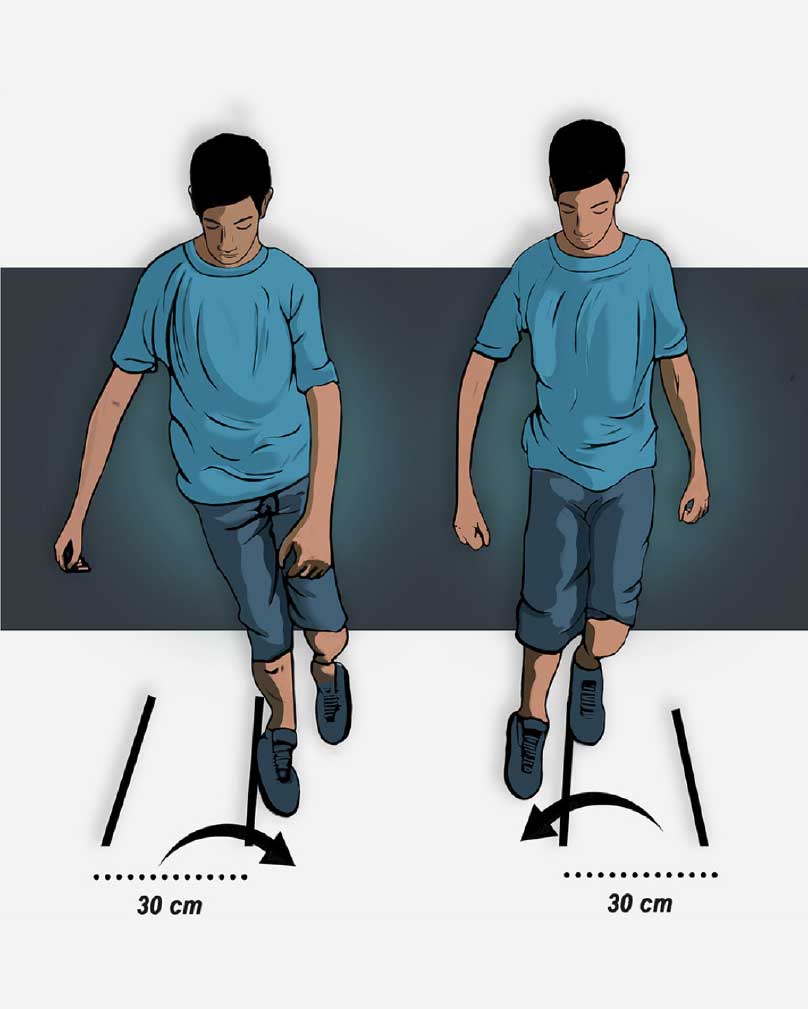
Side-hop test (Picot et al., 2022).
Literature sources:
- Doherty C, Bleakley C, Hertel J, Caulfield B, Ryan J, Delahunt E. Recovery From a First-Time. Lateral Ankle Sprain and the Predictors of Chronic Ankle Instability: A Prospective Cohort. Analysis. The American Journal of Sports Medicine. 2016;44(4):995-1003. doi:10.1177/0363546516628870
- Feger, Mark A. PhD, ATC; Glaviano, Neal R. MEd, ATC; Donovan, Luke PhD, ATC; Hart, Joseph M. PhD, ATC; Saliba, Susan A. PhD, ATC, MPT; Park, Joseph S. MD; Hertel, Jay PhD, ATC. Current Trends in the Management of Lateral Ankle Sprain in the United States. Clinical Journal of Sport Medicine 27(2):p 145-152, March 2017. | DOI: 10.1097/JSM.0000000000000321
- Fong DT, Hong Y, Chan LK, Yung PS, Chan KM. A systematic review on ankle injury and ankle sprain in sports. Sports Med. 2007;37(1):73-94. doi: 10.2165/00007256-200737010-00006. PMID: 17190537.
- Gribble PA, Bleakley CM, Caulfield BM, Docherty CL, Fourchet F, Fong DT, Hertel J, Hiller. CE, Kaminski TW, McKeon PO, Refshauge KM, Verhagen EA, Vicenzino BT, Wikstrom EA, Delahunt E. Evidence review for the 2016 International Ankle Consortium consensus. statement on the prevalence, impact and long-term consequences of lateral ankle sprains. Br J Sports Med. 2016 Dec;50(24):1496-1505. doi: 10.1136/bjsports-2016-096189. Epub 2016 Jun 3. PMID: 27259753.
- Picot B, Hardy A, Terrier R, Tassignon B, Lopes R, Fourchet F. Which Functional Tests and Self-Reported Questionnaires Can Help Clinicians Make Valid Return to Sport Decisions in Patients With Chronic Ankle Instability? A Narrative Review and Expert Opinion. Front Sports Act Living. 2022 May 26;4:902886. doi: 10.3389/fspor.2022.902886. PMID: 35721875; PMCID: PMC9204606.
- Tassignon B, Verschueren J, Delahunt E, Smith M, Vicenzino B, Verhagen E, Meeusen R. Criteria-Based Return to Sport Decision-Making Following Lateral Ankle Sprain Injury: a. Systematic Review and Narrative Synthesis. Sports Med. 2019 Apr;49(4):601-619. doi: 10.1007/s40279-019-01071-3. PMID: 30747379.
- Wikstrom EA, Mueller C, Cain MS. Lack of Consensus on Return-to-Sport Criteria Following. Lateral Ankle Sprain: A Systematic Review of Expert Opinions. J Sport Rehabil. 2020 Feb 1;29(2):231-237. doi: 10.1123/jsr.2019-0038. PMID: 31141438.
💚Do you need support with your workout, rehabilitation after injury or just want to feel more comfortable and healthy in your body overall? Check out our offer or book a free online consultation.⠀